All Activity
- Today
-
789bethncom1 joined the community
-
Gmncblog joined the community
-
789pgameapp1 joined the community
- Yesterday
-
Myhead joined the community
-
vnnohuitcom changed their profile photo
-
vnnohuitcom joined the community
-
NeitherHere started following mania and depression - are clusters a bi-product of bi-polar
-

mania and depression - are clusters a bi-product of bi-polar
NeitherHere replied to Monica's topic in General Board
Diagnosed c-ptsd, bipolar, bpd, take the book flip through the pages and point at something and i'm sure a doctors tried putting that label on my files. I was raised around hard drug use, extreme dv,psychological abuse, malnutrition, outright neglect, had a crippling liquor cns depressants addiction namely opiates and multiple cns depressants together i.e. handle of vodka with a bunch of opiates and barbiturates. Did 15+ years trauma therapy. I recovered from most of it but I still don't trust people as a rule of thumb. I've seen too much to blindly hand people trust. I've also had atleast 6 concussions and multiple critical heat/dehydration events. Atleast 3 of each of the above including loss of identity and consensus reality as well as having to relearn how to spell. My clusters started about 3-4 years ago. I was going through some massive betrayals and I was exceptionally pissed off. I mean like.. do some crazy crap pissed off. I was driving and my blood was boiling when out of no where I had my first attack. It was like the rage itself had manifested the clusters. I got past the stuff that had me so angry, made ammends but the clusters have haunted me since. I consider it gods gift. A persistent reminder that no one is allowed to piss me off like that unless I allow them too. I've survived much worse so why am I going to allow something to convince me that life isn't worth it when I've seen quite the contrary. I'm scared of death much more than i'm scared of misery. This cycle I've decided to weaponize my clusters to my benefit. Everytime it pisses me off its time to train. Everytime it gets me feeling hopeless i'm going to do intense workouts. If I so much as even think about death its running until I can't catch my breath. I've survived too much to let a headache to let me think life isn't worth it. On the contrary, I welcome the pain. Make me stronger. Make me harder to weaken. Its misery, theres days I dont want to be here about it, but thats my pain leaving the body. Thats my psychy cracking under load. It makes more sense for me to fortify than it does to lessen the load. That's not to say that I won't try to bust but if a car cracks a block of driveway you dont stop parking there you make the pad thicker. I will train my brain to treat these headaches as a personal attack that must be met with extreme prejudice. Harden the defenses. The diagnosis' are nothing more than labels trying to explain a history that is unexplainable. Those doctors did nothing but slap bandaids on the issues and teach me to be okay with the things that happened. I wish they would have made me angry towards the issues, taught me to harvest that pain and suffering for growth. None of what I endured is okay. It never was. None of those medications benefited me, all they did was allow me to stay weaker longer. Si vis pacem parabellum. -
j88mobi9 joined the community
-
kinglab started following mania and depression - are clusters a bi-product of bi-polar
-
mm88reisen11 joined the community
-
ccakhiatvcctv joined the community
-
sunwinteam1 joined the community
- Last week
-
mania and depression - are clusters a bi-product of bi-polar
Bibbers replied to Monica's topic in General Board
Yes, this is also a pet theory of mine. My husband has ECH and had a litany of trauma growing up from alcoholism and drug addiction in his parents, physical abuse, homelessness after leaving his home early, death of friends and close family as a young man. I just finished The Mindbody Prescription book, which is primarily about repressed rage and grief, and how it will present as pain in the body as a way of distracting the mind from its subconscious feelings. But what's more, it is absolutely possible for the limbic system to form neural pathways to the hypothalamus and cause autonomic dysregulation. -
mk8acc changed their profile photo
-
williamanderson started following Time Sensitive Action for Children with Headache Disorders
-
Thinkedubox started following Herbal Cigarettes
-
cm88betjuaravip changed their profile photo
-
cm88betcom changed their profile photo
-
c168lccom changed their profile photo
-
789clubcclub1 changed their profile photo
- Earlier
-
c168company changed their profile photo
-
mk8th changed their profile photo
-
qq8827com1 changed their profile photo
-
uk888org changed their profile photo
-
That’s actually something I’ve been curious about too. Even if herbal cigarettes are tobacco-free, the act of inhaling smoke itself can still be irritating and potentially trigger attacks for some people. Cluster headaches are often sensitive to strong smells, smoke, and changes in oxygen levels, so it wouldn’t surprise me if they could exacerbate symptoms. From what I’ve read and heard in similar discussions, many people with cluster headaches tend to avoid any type of smoke altogether, just to be on the safe side.
-
Thank you
-
I must of missed them, I've had 20-25% results with busting, I'm on the D3 regime all the time, I thinks its just good health to be anti-inflammatory, I also intermittent fast to keep inflammation and insulin spikes down. I tried a 96 hour fast at the beginning of this cycle, and so far I think its reduced overall attacks. I'll try anything during a cycle. But once its gone, I rarely even think about it.
-
One thing that many people have noticed is that when the tank gets below a certain level (half-full for some, one-third full for others), O2 loses effectiveness. With a regulator that goes above your usual level, you can increase the lpm to compensate for this. You didn't answer about D3 and busting (perfectly fine), but I'll just repeat that they make a big difference.
-
Jetpack Compose + Material13, Language Kotlin. I build in Antigravity.
-
I'll check that app out in the next few days. What framework is it? Also the iPhone thing I can relate to. That is why I usually stick to a web app so both android and apple are available without needing to build two apps but thats just my preference.
-
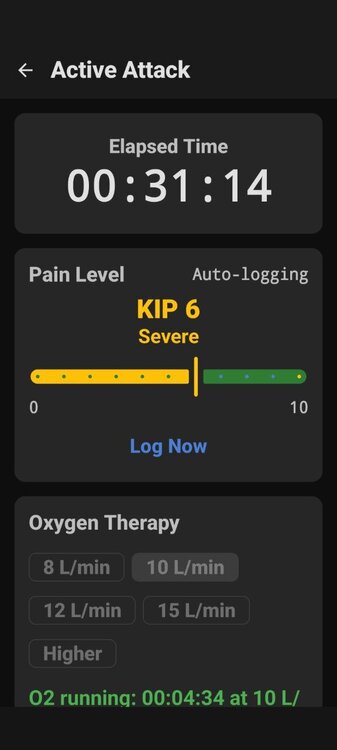
I hadn't loaded all the the data into the app yet, I only had a few actual live runs with it where O2 was logged, and then I was back loading attacks so that I could see a complete cycle. When doing so I realized that the past logged events didn't include O2 usage so it through the stats off. I fixed that, in the latest update. The new Stat averages 19.61 min per attack or 922 Minutes over 47. I had also corrected the calendar issues, added edit ability to past attacks (sometimes I forget to hit end) I'm just so happy its over. We already had the JSON export, but I added and tested an import in case you switch phones later, you can export out of current phone, load app in new and re import. No data loss. I ended up hosting it on Github as then when I push releases or add on's people can just update. There is also good notes on what app is all about along with ability to audit the code if your inclined. For $25.00 I get get it listed on the Play Store, something I might consider to get it to a larger community after I get feedback and see if this is an app people will want to use, then updates will be automatic. I did look into optimizing for Iphone, I figure it would take me an entire weekend (personally I am not a fan of Iphone) but I may consider it if like I said there is enough interest. Good news is that I will not allow advertising or charge a fee as I consider this my contribution to the community. https://github.com/MyDigitalFreedom/ClusterTracker/releases As far as optimizing O2, I can't say that I have been overly successful, What works one day, doesn't the next, as many know this beast just changing. My old manual records were harder to see any patterns. I'm hoping with the graphs I will get more insight.
-
Herbal cigarettes may be tobacco-free and nicotine-free, but they still produce smoke when burned, and that smoke can irritate the airways and potentially trigger coughing, wheezing, or asthma-like symptoms in sensitive individuals. “Herbal” does not automatically mean safe for the lungs. If you’re curious about the types available in the market, you can explore this list of herbal cigarette brands. However, even these product can still cause repiratory irritation, beacuse the main issue is the smoke itself, not the tobacco.
-
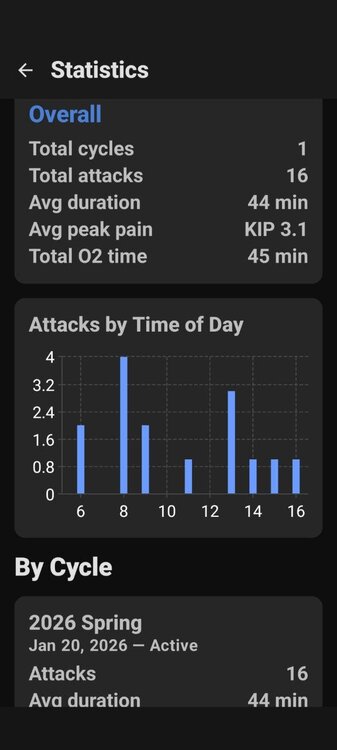
@Trent, I remember from some years back that you gave a lot of thought to optimizing your O2 usage, and you were dealing with some Canadian restrictions on equipment. An average attack duration of 44 minutes seems too long, and a total O2 usage of 45 minutes over 16 attacks seems quite low, so I'm curious about what's going on, and of course I am also curious about whether you are doing the D3 regimen or busting, both of which typically reduce attack durations. Since this isn't really the subject of these posts and you aren't asking for any advice, you don't have any obligation at all to answer . . . It just makes me curious about whether there's something that could reduce those longer attacks.
-
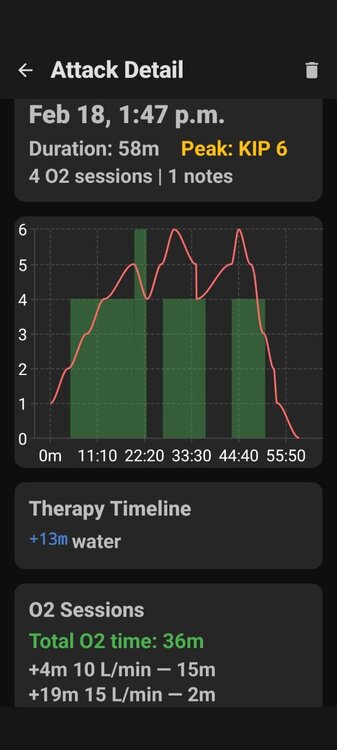
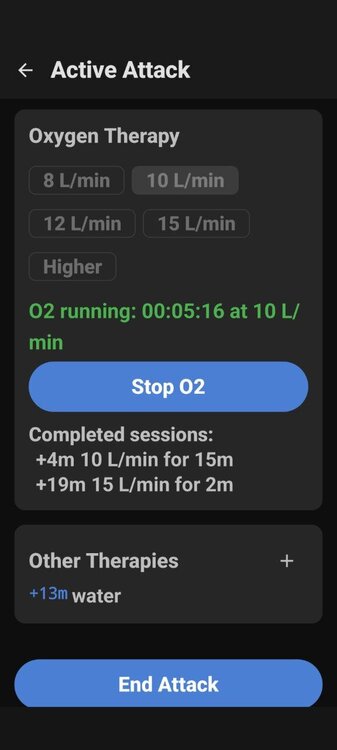
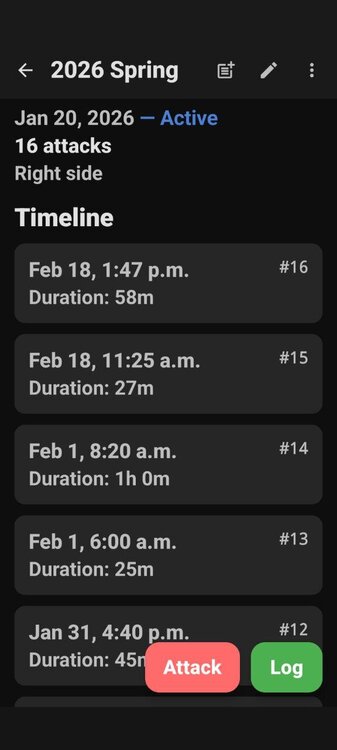
Here is some screen shots, also of note not available on i-phone. You can see where I thought it was going away, so I stopped O2, then quickly regretted that.
-
The above app is 100% hosted and stored on your own phone/tablet. No data is transmitted to anywhere else. I specifically built without Google play services for privacy reasons. Now to be honest I would not install a random app on my device without knowing where it came from. So my recommendation is to load it on a old phone you got kicking around and try it there first. It won't need a sim card or even to be up to date, and can be installed over wifi.
-
Its got some minor glitches I am still working out but here is what I built for myself. I use it to track cycles, attacks within the Cycle and the attack it self. If there is interest I will provide updates. The glitches I found where adding past attacks, the calendar was off by one day, so I choose one day ahead for yesterday's log date. I also want to add the ability to edit past attacks and notes. But otherwise working great. Provides good analytics for Cycles, and Attacks. Logs Pain, and O2 Usage and tie to local weather for increased data collection. Files can be exported into JSAN or CSV for medical or historical record keeping. The Notes can be for anything you wan to record, busting attempts, diet, D3 Regime tracking ect. Hope you all like it. https://github.com/MyDigitalFreedom/ClusterTracker/releases
-
Why is the D3 Regimen not common knowledge after all this time?
dhuddly replied to Bilal's topic in General Board
@Craigo Brother I mean what I say and probably literally with how I type lol. It hurt. And I enjoy reading your interactions and guidance in these forums. You obviously didnt mean to cut me like that because it's clear to me you really care for everyone here. I won't ever hold one reply or one response against anyone here. I appreciate what you say and I appreciate what you have said in the past on here. Your past forum chats are really good and caring. One of my favorites here so far lol. Probably why it stung but anytime you want to talk I'm also a phone call away or zoom call. CH is too important and shared between all of us here. -

Why is the D3 Regimen not common knowledge after all this time?
Craigo replied to Bilal's topic in General Board
@dhuddly and to all reading. After a sleep I feel I overstepped with my comments above so I wanted to offer an apology and make clear that's my stuff, not his and I should have chosen my words better. Sorry Dhuddly, hope you may be able to accept my apology. -
We should also specifically look at adding video features. Because as I have learned recently, all of us talk and type differently. We are from all walks of life. If there's been misinterpreting due to text lengths and formats then video is an option to help us differentiate things like crazy or delicate. Because when anyone lands here, it means that they are finally vulnerable enough to be here. For example, in video you guys would see me talk fast. It's my nature. But in text forums like this, I write very long replies. Not because I am long and slow or delicate. Lol for me it's literally an ADHD thing that's never slowed me down. If storage is an issue for video features then there are plenty of avenues we can use or explore. It also would allow for a healthier community experience because anytime you have a face and voice to connect to the text it paints the whole picture. Just some food for thought.
-

Why is the D3 Regimen not common knowledge after all this time?
Craigo replied to Bilal's topic in General Board
I can work with truck driver vocabulary and your grammar isn't that bad. Books and written to be read and videos to be watched, I'd love to check them out, please feel free to drop links here or send me a DM so I can go check them out. I just read The Headache, Tom Zeller Jr, episodic cluster sufferer and it was an absolutely amazing read. Welcome again to the community @dhuddly, if that's what you were after then certainly you are in the right place, there are some phenomenally good people in the cluster headache community, of that I can say for sure - and the reason I reckon I will be back in Chicago come October for this years conference! -
Why is the D3 Regimen not common knowledge after all this time?
dhuddly replied to Bilal's topic in General Board
Craig no offense taken. And sorry if this comes across as defensive, I am aware of what you describe, I am also aware that I don't talk how I type and I don't type how I talk. I can understand why you are saying this to me but I would suggest maybe checking out some videos I made during covid. They have nothing to do with cluster headaches and only connect in a way that let's me know that the ch didnt take all of me and I survived. Beyond that the research I've compiled was a direct result of me fighting me way back so through the most traumatic and painful time in my life. I am described as a blunt person long before this. Through years of some of the same things you listed and can appreciate why you'd feel led to make sure I'm not out of my mind. I have no expectations from this forum. I am here because I needed to find community. People don't get through this level of trauma alone and sounds like you understand that. You can see those videos on TikTok. They've been there for years. I talk alot in them. The way you read my text in these forums will I guess allow you to understand that long responses, run-on sentences is kind of my thing. Even since MySpace I was aware that some people misunderstand how I type sentences in text. Just like this reply is too long. Its just something I've accepted decades ago. In person, I am the type that is comfortable delivering hard messages to people and that translates to caring. And that is definitely something we share Craig. Oddly enough, the first thing I did as far as treat myself to normalcy after ch was to write two books that I began back in the videos im talking about. Years of me being me brother. I have the grammar of a 10 year old and vocabulary of a truck driver. But that doesn't mean I'm out of my mind brother. -

Why is the D3 Regimen not common knowledge after all this time?
Craigo replied to Bilal's topic in General Board
Hi @CHfather and @dhuddly. Sorry you find yourself in our company there dhuddly, I haven't been on past couple weeks with some life changes I alluded to above and a number of projects on the go. I would appreciate links to studies you've read, always keen to expand my knowledge of the vitamin D3 literature. Here are the studies and their findings relating to the dopaminergic system in CH published last year for your reading and interest. What I would say above and beyond these studies, the work that has come out over the past number of years in CH space makes it fairly clear that between the active bout periods in episodic CH, the patient does not return to a normal baseline, the attacks may stop but there are perturbations that extend into the interictal periods that give me some level of assurance that I am doing the right thing for myself in terms of staying on the anti-inflammatory regimen 365 days of the year. I also hope that in doing so, I am providing an additional level of protection against developing other disease. I have more recently revisited Dr. Gominak's work (a contributor in part to the regimens inclusion of the B-Vitamins) and believe another reason for the regimens efficacy relates to vitamin D3's influence on the composition of the gut microbiota and the maintenance of epithelial tight junctions. Given nearly every cell expresses the VDR and the lack of formal studies in CH, it would be impossible for us to confirm Pete Batcheller's original hypothesis as to its precise mechanism of action (and as you mention, partial or non-response) but I think he is on the money with the umbrella thinking that it's underlying mechanism is the up and down regulation of genetic products which have the VDR sequence in their promoter / enhancer or silencer regions on DNA. Dysfunctional mesocorticolimbic circuitry in cluster headache. Ferraro et al. (2025) This fMRI study used a "Monetary Incentive Delay" task to probe the mesocorticolimbic dopaminergic pathways. Chronic CH (cCH): Patients exhibited blunted activity in the Ventral Tegmental Area (VTA) - a central dopaminergic hub - during reward anticipation. They also showed an imbalance in the pathway between the VTA and the medial prefrontal cortex (mPFC). Episodic CH (eCH): Patients showed intact VTA responses but abnormal mPFC activity, which the authors suggest may be an early sign of emerging dysfunction in the VTA-mPFC dopaminergic pathway. Conclusion: The study suggests an abnormal dopaminergic state in chronic patients that is distinct from affective disorders (depression/anxiety). Uncovering the neurological substrates underlying restlessness in cluster headache - A functional MRI study Chen et al. (2025) This study investigated the neural correlates of restlessness/agitation, a core clinical feature of CH. Substantia Nigra (SNpc): Patients experiencing restlessness showed increased functional connectivity between the Substantia Nigra pars compacta (SNpc) - a dopamine-producing nucleus - on the pain side and the Locus Coeruleus (noradrenergic) on the non-pain side. Frontal Inhibition: The study found decreased connectivity between the pain-side SNpc and the superior frontal gyrus, suggesting a disruption in top-down inhibitory control contributes to motor restlessness. Neurotransmitter Imbalance in Cluster Headache: A Systematic Review of Mechanisms and Therapeutic Targets Pellesi et al. (2025) This review aggregates data from multiple biochemical studies regarding dopamine levels in CH. Platelet Levels: Citing D'Andrea et al. (2006), the review notes that platelet dopamine levels were significantly higher in patients with episodic CH during both active bouts and remission compared to healthy controls. Plasma Levels: Citing D'Andrea et al. (2017), the review reports that patients with chronic CH exhibited higher plasma levels of dopamine compared to controls. Cerebrospinal Fluid (CSF): Citing Strittmatter et al. (1996), the review notes that CSF levels of dopamine were not significantly different between CH patients and controls, though norepinephrine was reduced. Autonomic dysfunction in patients with episodic cluster headache during remission period López-Bravo et al. (2025), This study summarizes previous biochemical findings in CH. It cites D'Andrea et al. (2017) regarding Abnormal Tyrosine Metabolism: Chronic CH patients show increased levels of dopamine and its precursor tyrosine in plasma. The authors interpret this anomaly in tyrosine metabolism as a potential predisposing factor for the chronification of episodic CH. Thesis: Felicia Jennysdotter Olofsgård (2025) Jennysdotter Olofsgård (Thesis) Genetics: A meta-GWAS identified WNT2 as a new risk locus for Cluster Headache. The author notes that WNT2 is known to be involved in dopaminergic neuronal development. What is seldom discussed in our community is the psychological and personality dimension of CH and how that relates to this topic. Kudrow and Graham were notably candid in the 1970s. I hesitate to be quite so direct, yet many of the personality characteristics they described feel uncomfortably familiar, as though my name might as well have been written beside them. If I may delicately say @dhuddly, from your posts and your manner of written expression, you come across as highly intelligent, thoughtful and kind. You have also mentioned being a full stack developer (I saw that response on a possible CB app - thank-you!), someone your friends describe as operating at extraordinary speed. I want to be clear that I am not attempting to analyse or explain you, rather, those observed qualities deeply resonate with me and provide a useful reference point for describing how I have come to interpret similar tendencies in my own life, over-achievement, high intelligence, tendency to work at a million miles an hour to name but a few. So... here's my story and my take on those qualities in the context of my life journey and CH. My father died before I was born. Throughout childhood I struggled to understand, let alone regulate, the emotions associated with that absence. In adolescence this unresolved grief drifted into substance abuse. Later, the same undercurrent appeared to transform into an intense drive for achievement, knowledge, and ultimately explanation. A life organised around such a pursuit rarely tolerates stillness. Pausing to enjoy simple pleasures can mean confronting emotions one has never properly learned to process. I am still learning how to do that. My sense, shaped by both experience and reading, is that unprocessed anger, grief, and guilt can sustain a chronic autonomic bias toward fight or flight, with downstream effects across our physiology. Viewed through that lens, it is perhaps unsurprising that my nervous system, which has otherwise been remarkably resilient, shows points of vulnerability. I cannot claim definitive evidence that CH, or another unique and uncommon disorder I am afflicted with - vocal cord dysfunction, arises from such experiences. This remains an interpretation, not a conclusion. The closest conceptual framework I have encountered is found in the work of Dr Allan Abbass, particularly his writing on overcoming emotional resistance through Intensive Short Term Psychodynamic Therapy. I feel his work and this topic deserves more discussion, as confronting as these topics can be. Link. Anyway, I pray I have not overstepped and I welcome you here with open arms. I am glad to connect. Craig. -

Cluster Headache Awareness Day Chat
Craigo replied to eagleswings's topic in Advocacy, Events and Conferences
See you there- 1 reply
-
- 1
-

-
If we could compile a detailed list of what the app would need to do I could have us a fullstack app in no time. I can do several frameworks but enjoy NextJs the best since it is web based. No need for playstore and apple when you use NextJS. This website here is great though and could easily be converted. If you mean a native app, I would offer some positive pushback why keeping it web based can reach more people though. If you mean social media type of app with various functions and more dynamic than static, I have a couple MVP's collecting dust we could use. Whatever you decide though please know I'd definitely volunteer my skills and knowledge for the mission.
-
Hey folks, my name is Knyaz, who want to make more easy our lives and i have created "Migraine Tracker: Relief Pain" app which is serve for us. I need your help and feedback what i should add or delete pelase help me. App link: https://apps.apple.com/pl/app/migraine-tracker-relief-pain/id6755659669 WebSite: https://www.migraine.live/


.thumb.jpg.20e1d9ca766e9dad605483fcfa5efc87.jpg)




.thumb.jpg.5fbf5b94a439b99ad119c32de27d000b.jpg)



.thumb.png.f03e7799aff362d7d15945340ebb6f1e.png)




.thumb.jpg.24dde7ef3152d6d31b9546e3fec3b26d.jpg)