Leaderboard
Popular Content
Showing content with the highest reputation since 09/21/2025 in Posts
-
Hi all. I wanted to build on a post couple of months back that mentioned this early 2025 study in Annals of Neurology which found that Oncostatin M (OSM) was significantly elevated across all forms of cluster headache (CH), episodic in cycle (ECH), episodic in remission and chronic (CCH) when compared with controls. Distinct Alterations of Inflammatory Biomarkers in Cluster Headache Lund, N. L. T. et al. Annals of Neurology. 2025 https://pubmed.ncbi.nlm.nih.gov/39981939/ Interpretation: Findings show that the immune system is altered in all 3 states of cluster headache compared with controls. Oncostatin m was elevated, constituting a promising target for future studies. The distinct alterations between episodic and chronic cluster headache are striking and urges further research of the immune system in cluster headache to better understand its potential role in prediction of disease activity and treatment response. OSM belongs to the interleukin-6 family of cytokines which are signalling molecules released by cells to facilitate communication within the immune system and the body, acting as messengers and binding to receptors on other cells to trigger responses like inflammation, cell growth and immune cell activation. OSM is produced mostly by activated monocytes and macrophages along with T-cells once the immune system is already engaged. Triggers include microbial products such as lipopolysaccharide acting on toll-like receptors, upstream cytokines like IL-1β, TNF-α, and IL-6 as well as T-cell activation itself. In other words OSM typically appears as a second-wave signal once innate and adaptive cues are already active. After its release OSM signals through receptor complexes that require gp130 subunit, a shared hub for the IL-6 family. OSM pairs gp130 with either OSMR or LIFR receptors which activate Janus kinase enzymes (JAKs). JAKs phosphorylate STAT3 (signal transducer and activator of transcription 3) and activated STAT3 then enters the nucleus to upregulate genes for chemokines, adhesion molecules and matrix metalloproteinases. Short-term controlled activation of this pathway is essential for tissue repair but sustained persistent activation may lead to detrimental effects including weakened barriers, leukocyte recruitment and ongoing systemic inflammation. In Crohn’s disease and ulcerative colitis OSM has been shown to drive stromal activation and barrier dysfunction and high levels of OSM are a predictor of poor response to anti-TNF-α therapies. The CH study by Lund and colleagues suggests a similar kind of hard-to-quiet inflammatory program in the cranial milieu of CH patients regardless of whether or not they are in active cycle. So what may drive the persistent upstream activation that induces OSM in the first place? This wasn't discussed in the article but one source that may deserve attention is the emerging gut-immune-brain axis. As explored in my earlier post, a growing body of literature in migraine describes altered gut and oral microbiota, reduced microbial diversity, links to markers of intestinal hyperpermeability and bacterial endotoxin exposure as causative agents in migraine pathology. While migraine and CH are distinct disorders both share neuroinflammatory components, cytokine involvement and respond to many of the same treatments, is it reasonable to ask whether dysbiosis may help maintain the triggers that induce OSM expression? And if so what implication does that have on future treatment strategies for CH? And where might the Vitamin D regimen fit into this picture? The active form of Vitamin D, calcitriol, binds to the vitamin D receptor in immune and barrier cells and influences the expression of hundreds of genes. It suppresses NF-κB and MAPK signalling, promotes regulatory T-cells and IL-10 and strengthens barrier integrity by upregulating tight junction proteins in epithelial and endothelial cells. Building on Pete Batcheller’s hypothesis, maintaining sufficient blood levels of Vitamin D3 may help downregulate some of the upstream drivers of OSM expression while counteracting OSM’s disruptive effects on barrier function. Supporting this idea, work outside the headache field has shown that calcitriol can shift macrophages from an M1 pro-inflammatory state toward an M2 reparative state, reducing the production of OSM, TNF-α, and IL-6. A balanced view is important. The 2025 study identifies OSM as a persistent signal and points to specific differences between chronic and episodic CH. It did not identify a cause and it did not test interventions. The migraine-microbiome literature suggests dysbiosis as one possible upstream driver but translation to CH is yet to be explored. Other papers from this author on CH for your interest. https://pubmed.ncbi.nlm.nih.gov/?term=Lund+NLT&cauthor_id=37667192 Includes an article titled "Current treatment options for cluster headache: limitations and the unmet need for better and specific treatments-a consensus article" which concludes "We find that there is a great and unmet need to pursue novel and targeted preventive modalities to suppress the horrific pain attacks for people with cluster headache."4 points
-
Hi CHfather - thanks for stopping in. This is the first case series I am aware of looking at a gepant and CH, in this case Qulipta / Atogepant. There is a trial looking at Nurtec / Rimegepant as a preventative therapy for CH. Ubrelvy / Ubrogepant is more an acute treatment owing to short half-life makes preventive use impractical and may not act quickly enough for acute CH attacks. I haven't read anything about the third generation gepant Zavegepant, again an acute treatment via nasal spray. I haven't really followed patient feedback on any them tbh. I think this case series, if anything, may provide some context for clinicians considering where to next for refractory CH patients non-responsive to other treatments, including anti-CGRP mAbs like Emgality / Galcanezumab - this suggests that atogepant may be worth a try. I imagine there may be a tendency to think if a mAb hasn't previously worked or stopped working as was the case for one of the cases, a gepant is unlikely to either. That being said, ya'll know I have had success with the vitamin D3 anti-inflammatory regimen and my personal view would be to exhaust the patient led treatments options that we have (busting + regimen) paired with abortives (oxygen and more recently DMT) before considering one of these new treatments because I am somewhat adverse to risk and there is no long term clinical data on their safety. For refractory patients for whom my heart truly aches, this may offer some hope - still, an early signal and a small case series.3 points
-
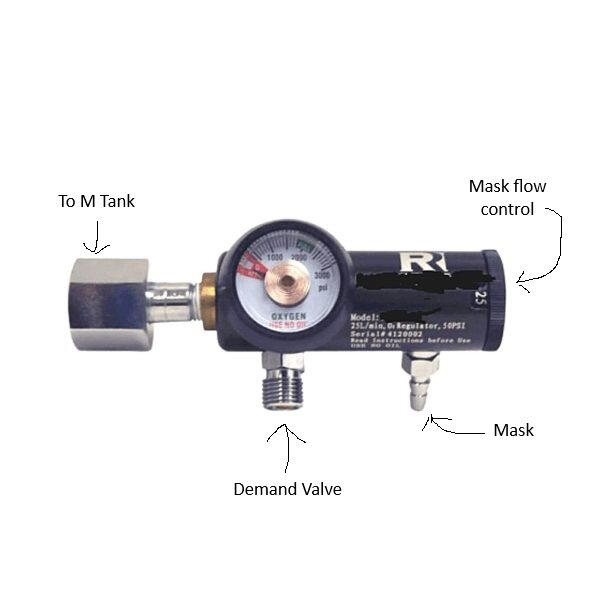
I'm attaching a pic to illustrate parts of the regulator. When you turn the M tank on, the demand valve will be charged and ready to use. The mask flow control has no effect on the demand valve. You will leave it on "0" unless you use the O2 mask rather than the demand valve. You will need an adjustable wrench of sufficient size to attach the regulator to the tank and the demand valve to the regulator. Ensure the tank valve is closed before swapping regulators.3 points
-
Can atogepant be a preventive treatment for cluster headache?-Insights from a case series Catarina Serrão, Filipa Dourado Sotero, Linda Azevedo Kaupilla, Isabel Pavão Martins Published in Headache on October 3, 2025 Link: https://doi.org/10.1111/head.15066 Abstract: Cluster headache (CH) is a disabling primary headache disorder with limited therapeutic options. Calcitonin gene-related peptide (CGRP) is known to be involved in CH pathophysiology; however, except for galcanezumab (300 mg) in episodic CH, anti-CGRP monoclonal antibodies did not reduce CH attacks in randomized clinical trials. Atogepant is an oral, small-molecule, CGRP receptor antagonist, which is approved for the preventive treatment of migraine. Here, we describe four case reports of CH (two episodic CH and two chronic CH), unresponsive to previous prophylactic treatments, who responded to daily atogepant (60 mg). Chronic CH cases were refractory to subcutaneous galcanezumab. In one case, a reduction to atogepant (30 mg daily) resulted in recurrence of headache attacks, which subsided on reintroduction of the initial dose. No serious adverse effects were reported. Despite the limited number of cases and the open retrospective design, our case series suggests atogepant as a possible prophylactic treatment for CH. Further research on CGRP signaling in CH and the implementation of well-designed clinical trials are necessary.2 points
-
In the US, the brand name for atogepant is Qulipta. In the EU, I think it's Aquipta. @Craigo, thank you for this (and for all your other great contributions to substantive knowledge about CH)! I notice that Ubrelvy and Nurtec are both also gepant formulations. Might we imagine that they would also help (it seems from the abstract that the contrast in this study is with galcanezumab (Emgality))?2 points
-
Ok folks.....I can't take credit for finding the following and it was so cheap I thought it was a scam. So.....I ordered one before spreading the word. It came today and appears to be legit. Demand valve and hose for $50 US. Brand new, in the box. Ebay Link2 points
-
If you have significant pain all day, and the attacks that seem like CH are "bursts" as you write (which I think of as briefer than a typical CH attack), and if a triptan doesn't help, it seems possible to me that you might have one of the CH "lookalikes," some form of hemicrania, maybe paroxysmal hemicrania (Paroxysmal Hemicrania: Causes, Symptoms & Treatment) or hemicrania continua (Hemicrania Continua: Causes, Symptoms & Treatment). I'm just guessing here: you can look to see how well the symptoms match. Unlike CH, hemicrania is generally not responsive to triptans or oxygen (or busting, except for some brief relief of maybe a day or two). So one test would be to take the medicine that treats hemicrania, Indomethacin. Another would be to try oxygen. As I say, I'm just guessing here. Sometimes people "try" Indomethacin, but the dosage isn't enough, or it's not continued long enough, to get a real test. This is the recommendation from the International Headache Society: "In an adult, oral indomethacin should be used initially in a dose of at least 150 mg daily and increased if necessary up to 225 mg daily. The dose by injection is 100-200 mg. Smaller maintenance doses are often employed."2 points
-
ABSTRACT: Classic psychedelics and the gut microbiome interact bidirectionally through mechanisms involving 5-HT2A receptor signaling, neuroplasticity, and microbial metabolism. This viewpoint highlights how psychedelics may reshape microbiota and how microbes influence psychedelic efficacy, proposing microbiome-informed strategies such as probiotics or dietary interventions to personalize and enhance psychedelic-based mental health therapies. Psychedelics and the Gut Microbiome: Unraveling the Interplay and Therapeutic Implications https://pubs.acs.org/doi/abs/10.1021/acschemneuro.5c00418 A fascinating new view-piece synthesizing the current literature exploring psychedelic / gut / microbiome interaction in the context of depression. Wang and colleagues emphasise that "the baseline composition and functional state of the microbiome can shape psychedelic pharmacology and therapeutic efficacy, while the psychedelic experience itself can remodel the gut microbiome in ways that influence ongoing physiological and psychological adaptation." At the cellular level they note psychedelics suppress the production of pro-inflammatory cytokines IL-6 and TNF-α through 5-HT2A receptor-mediated inhibition of NF-κB signalling: "this immunomodulatory action establishes an anti-inflammatory milieu that favors the growth of beneficial commensal bacteria." Compounds such as psilocybin and DMT "reduce pro-inflammatory cytokine expression and enhance epithelial barrier integrity, promoting the expansion of anti-inflammatory taxa." They note, the microbiome is not a passive bystander: "gut bacteria express a variety of enzymes capable of biotransforming these substances, thereby shaping their pharmacokinetic profiles. For instance, Bifidobacterium species have been shown to affect the metabolism of DMT, potentially altering the intensity and duration of ayahuasca experiences. Similarly, in vitro studies have identified bacterial strains that dephosphorylate psilocybin into its active form, psilocin, suggesting that individual differences in microbiota composition may underlie variability in therapeutic response." Wang et al. refer early human data noting that "although human studies remain limited, early observations suggest that psychedelic treatment may be associated with alterations in fecal microbial diversity in patients with depression." These observations support what the authors call a "systems-level perspective of psychedelic therapy - one that encompasses not only neural targets but also immunological, endocrine, and microbial domains." The article is behind a paywall, send me a message if you'd like a copy of the article. For more reading the article cites this paper "Seeking the Psilocybiome: Psychedelics meet the microbiota-gut-brain axis" https://pmc.ncbi.nlm.nih.gov/articles/PMC9791138/ In the context of CH, with new evidence of persistent immune-inflammatory activity suggests psychedelic therapy not as acting solely on the brain but by potentially intersecting with the upstream gut-barrier-immune processes that maintain systemic inflammation that are now attributed as a causative agent in migraine. The paper also goes some way to positing a possible reason for the variations we see in busting efficacy. This area of research is fascinating and I think the piece provides a further and new angle as to the role gut health may play in CH alongside recent findings in migraine although there is much road to travel before we have any concrete evidence of this. Still mulling my thoughts, all I offer here is a view - always interested in yours. With respect, Craig.2 points
-
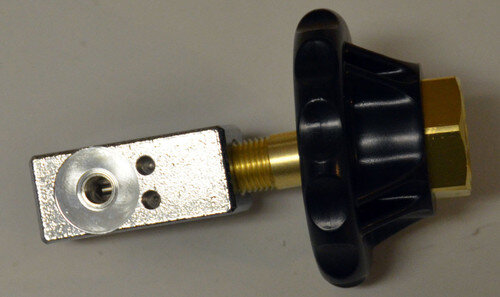
One of the issues we as CH O2 users has been when we have both M and E tanks available to use. The M/Welding tanks use a CGA540 connection, and the E tanks use a CGA870 thus preventing swapping regulators between the two. While I've known of an adaptor that allows you to run M tank regs on E tanks, I've only heard talk of a device that allows to reverse, the ability to use a E tank reg on a M tank. Until now, I didn't think such an adaptor could be sourced, but I finally found it and have tested it myself. It works!! There is a nonstandard seal requirement, but that's easily met. You simply order the thick seals linked below and use them in place of the standard brass/rubber seals we normally use. I have no financial connection to these items, and this is for informational purposes only. You be the judge if this set up is right for you. The adaptor. The seals.2 points
-
I think I have found a better deal for you. HERE This option will give you what you need plus a barb fitting for the mask as well so you can use either. Glad to help.2 points
-
Interesting, thanks for posting this. My Neuro has prescribed this for me at 60mg. I’ve not started just yet as I’ve been having some success with busting with 5-MeoDalt. Down to 1 attack per week and low pain shadows between. I was considering adding this layer on top. The cgrp blocker side effects of constipation and hair shedding give me the fear also :/1 point
-
1 point
-
TUESDAY NIGHT October 7 at 7pm ET During the session, you’ll: ● Understand how gammaCore works to treat cluster headache, including the science behind vagus nerve stimulation and its role in regulating pain signals. ● Learn strategies for incorporating gammaCore into your care plan and understand when and how to use it effectively. ● Have the opportunity to ask questions during a live Q&A session. Register Now: https://us06web.zoom.us/meeting/register/SrvzB0d4RoiK4Dz8ITjvrQ1 point
-
1 point
-
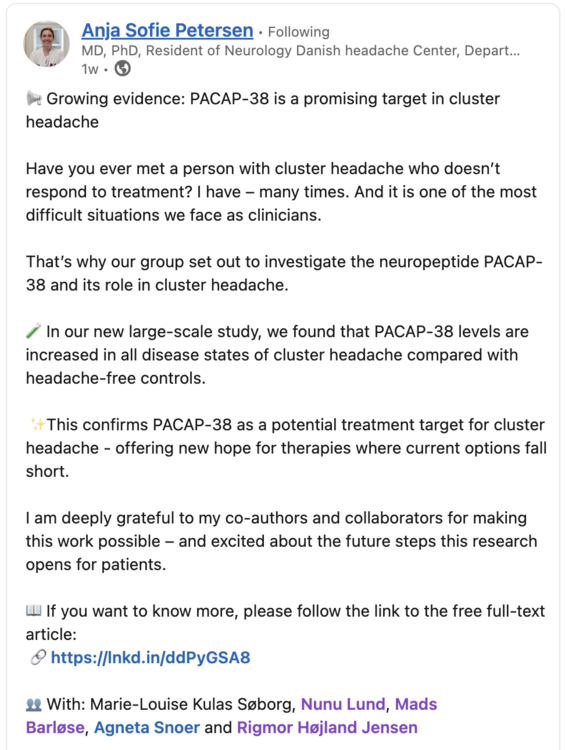
PACAP-38 in Cluster Headache: A Prospective, Case–Control Study of a Potential Treatment Target Marie-Louise K. Søborg, Nunu Lund, Agneta Snoer, Mads Barloese, Rigmor Højland Jensen, Anja Sofie Petersen Published in European Journal of Neurology on September 26, 2025 Link: https://doi.org/10.1111/ene.70341 Abstract: (partial selection) This large-scale study demonstrated increased PACAP-38 levels in all disease states of cluster headache compared to headache-free controls, strengthening the hope of a possible effect of PACAP-38 targeting treatments in future trials. The lacking correlation between PACAP-38 and CGRP levels should be interpreted with caution and needs to be investigated in future studies.1 point
-
Here is a screenshot from one of the authors posts on LinkedIn. The research coming out of the Danish Headache Center is outstanding, I have recently shared the findings of their paper identifying the distinct cytokine profiles that distinguish eCH from cCH and also found that Oncostatin M was elevated in all 3 CH states.1 point
-
Wow, that's terrible, sorry to hear it! If your neuro wasn't a headache specialist, well those are the ideal ones you want to see - it can be quite the long wait to get an appointment with one though, and that seems pretty universal, no matter what country you reside in. Last I checked, verapamil is known for lowering blood pressure, and is even prescribed for treating high blood pressure, so I wouldn't imagine your high blood pressure to be a verapamil side effect. I'll leave the T syndrome (or did they test for "T series"?) abnormality for others who may know about it. Sumatriptan injections have historically been prescribed in too high of a dose, specifically 6 mg, whereas doses of 3 mg (or even 2 mg for those such as myself), are plenty effective at aborting cluster attacks if caught at onset. It could be worthwhile to let us know what kinda sumatriptan and verapamil doses you have been prescribed - if you've been issued the big dose 6mg Sumatriptan (which I would have to think would increase risk of side effects), there are ways to split those injections:1 point
-
Hi @philiph, Magic mushrooms Busting dosage: typically in the .5g to 1.5g (dry) range. Reactions: Tripping, during the bust, then often relief from CH following, but also brace for possible 'slapbacks' (increased CH activity for a day or two). How long it takes varies, with 3 busting doses spaced 5 days apart an often successful protocol (for episodics anyway). It works for an impressively high percentage of us, but not 100% of us. DBS anecdote: One chronic member here had the DBS with no success, then eventually tried the mushrooms and got some very significant, sustained relief. The Blue 'NEW USERS - PLEASE READ HERE FIRST' banner at the top of the page links to more busting info.1 point
-
Usually Amazon has some, but it appears that right now that none are available there. You can configure one with a DISS fitting at WT Farley Here. E tanks regs are easier to source. I've also found an adapter that may work but am waiting on the proper seal to make sure its something i can recommend. There may be others but ATM I can't locate any. Ill keep my eyes open.1 point
-
This link for it that I received in an email functions for me: https://thethirdwave.co/webinar-cluster-headaches-and-neurological-disorders/ If it's still not working for you, maybe trying it in a different browser or something might be worth a shot?1 point
-
It was again an awesome time and great to se it growing over the few short years I have attended. Many more Doctors Authors and Vendors. Most of all a bunch of fun happy clusterheads from literally all over the world. Hope you all can make it next year.. Bring a friend and leave with 100 new ones.1 point
-
I appreciate i am very late to this conversation but I just want to drop in that red bull is now a key part of my armoury the moment the dreaded knock kicks in. I will post a detailed synoptic of my experience in coming days but for anyone suffering right now, seriously consider taurine. To me it's a life saver but I do have to say we are all different and some of us have intolerances and other complications so do be conscious of your personal needs. But if you don't have an issue with caffeine and taurine give it a go. Pour on lots of ice and gulp it freezing cold so it hits the back of your throat which is the nearest you can get to your pituitary gland without poking a hole in yourself. The cold soothes the brain and the taurine does some magic and at least dulls the agony. X1 point
-
I suffer from cluster headache episodes. They happen every 10 years or so and last up to 9 months with frequent attacks. Home-based oxygen therapy works for me (fortunately) to abort attacks. But what worked for me even better is scuba diving at relatively deep depths. I discovered this by accident a few years ago as I was preparing for a 120 feet dive on regular air. I had geared up and was preparing to dive in when an acute attack started. I was in month 3 of the episode and my morale had been eroded by the frequency and violence of the attacks (at that time, my physician had refused to supply me with home-based oxygen treatment - she was afraid I would start a fire!). We had been planning the dive for days and I thought to myself: "Screw that... I'm going in.". While the first few minutes were made quite difficult by the pain, I started feeling better at 80 feet and the attack vanished when we reached 120 feet. At first, I though this was a coincidence. But as we repeated the 120+ feet dives over the next 4 days, something unexpected happened: the episode was aborted and I was pain free for years afterwards. After talking to my neurologist about this event, he confirmed that there were more reports of busting an episode with diving at these depths. He also explained that he prescribed hyperbaric chamber treatment at simulated depths of 60 feet for cluster headache sufferers. He also explained that at the depths we went to, the oxygen concentration is almost 5 times higher than at surface level (approx. pO2 1.0 ATA at 125 feet vs 0.21 ATA at surface). This was the equivalent of a mammoth O2 treatment. I don't suggest here that anybody go out there and try this. Diving at these depths require special training and certification. But if you are a diver who is qualified and who suffers from cluster headaches, consider it. But make sure that you are comfortable at those depths (i.e. not anxious) and that your buddies are aware of your condition and what you are attempting to do. Frederic1 point
-
I am a dive instructor who started getting chronic cluster headaches that only responded to very high doses of steroids and of course you can’t stay on them long-term but over a decade ago I concluded that if 100% oxygen at sea level was effective in aborting an attack certainly should be helpful under pressure And then there’s other physiological reasons that are likely and I’m just guessing at that I don’t even want to elaborate on at the moment but I will say that I had to sell my house and become a professional diver in order to prevent attacks however I have to dive every 72 hours. I am not going to get into the details of my dive profiles because they’re totally irresponsible and not some thing I would recommend to anyone especially as an instructor but I do a lot of deep solo dives which buys me more pain free time and I feel like I am able to sleep otherwise I can go up to five days without sleeping And I don’t think that there’s any reason to go to the depths I go to I mean they’re approaching oxygen toxicity and I’m diving on air and most people wouldn’t be able to go that deep on air because they would run out doing deco stops or get so narced they can’t function. I am a very small female with great lungs and my air lasts forever but still I do this solo obviously because I would never risk taking someone with me. I am lazy and dictating and hopefully anonymous but I will say that I have never never had an attack underwater or within 24 hrs of a deep dive. Other headaches yes including sinus barotrauma or reverse blocks above the eyes that feels strikingly similar at surface to a cluster but resolves within minutes. I have destroyed my back and all of my disks are permanently herniated so I have to gear up in the water and I am prone to tension headaches but I’ll take a tension headache every fucking day over a cluster not that a tension headache is pleasant but for me the most likely cause of a headache from diving would be Probably from CO2 when I’m fighting a current and I think a lot of people get those and they think that’s bad I shouldn’t be diving but what you should be doing is diving without exertion to a depth that is at least 60 feet without stress and for a non diver I would not necessarily even suggest taking up diving unless you get one on one instruction I will occasionally take a max of two students if they beg to be taught together but training standards are just awful (says the lunatic solo diver who will certainly not return from a dive eventually but I am fine with that) I need to go deeper to get the longer-term affects and I hesitate to even say that and certainly am not recommending solo dives but in my case it’s a different situation. I know a lot of people who can Completely rid themselves of an attack it as little as 60 feet I prefer to go well beyond recreational limits because I guess I’m partly suicidal at this point and I just love it I feel like a human being for days afterwards. I’m tired but I love being tired because otherwise I won’t sleep for days. For years I have been interested in writing a much more rational approach to treating cluster headache‘s for divers and trying to get into some of the physiological responses that most of us experience in ideal environments (talking temperatures current etc.) that I am certain are benefiting us but I believe it’s much more than just the increased metabolization of oxygen and think it’s the shunting of blood from the extremities to the core, vasoconstriction but also by lowering of the body temperature in general and I am truly believe there’s one other element but I’m trying to get a neurologist who is a scuba diver to go on the record and discuss this with me and they’re reluctant. I am as well because I don’t want a bunch of people going out and getting certified especially by these shops that take eight students per instructor and you’re not trained at all you are not a diver at the end of those you might get a certification but you shouldn’t because no one‘s been even watching you and you certainly don’t have time to master any skills and it’s really important to have good trim and neutral buoyancy and good control he a very confident diver before you can even start thinking about treating your cluster headache and you might end up causing all kinds of problems that will result in other types of headaches or sinus barotrauma‘s that mimic very bad pain that could be confused with a cluster headache as I said there’s been a few people who’ve spoken about experiencing one as soon as they surfaced and I am skeptical of that and I suspect there might be something else going on there’s a lot of reasons diving can give you a headache all of them should be avoidable but in my case I definitely get some tension headaches I should be diving with a much smaller cylinder because I weigh 90 pounds I almost feel like there should be a recipe for every individual cluster headaches suffer you can’t just say y’all go diving although I would like to I’m very tempted to I feel like it’s reckless if you’re already a diver and been diving for a long time And you are fearing getting a cluster headache at depth I can say on the lives of my dead family members this will not happen. It Is the only situation in my life in the last 20 years where I haven’t had an attack the only one and I am chronic didn’t start chronic I started as episodic and I did respond initially to some medications but I had a standing order at my local emergency room for IV steroids followed by 60 mg of prednisone for five days and then 50 mg for four days and basically a really long taper so I start and end in about a month and they would allow me to do that every other month which is rare most doctors won’t let you do that often at all and I’ve been doing it most of my life And it also makes me nervous to sound like I am suggesting to people that they exceed recreational limits. I am straddling a threshold that will eventually lead to me not coming back from a dive but at this point in my life it is the only thing I live for it’s what makes me functional happy and most people have no idea. I don’t tell people I have no reason to tell people and I am not someone who wants sympathy definitely don’t want pity however I do want the ability to do whatever the hell I want and unfortunately at this stage of my life what I want to do is not some thing I would ever recommend anyone else does and there’s no reason to for probably 99.9% of cluster stuffers you just don’t need to do anything close to what I do you can dial it way back and, be safe, smart and conservative and have good success but if you’re just vacation diving this is not going to help you beyond the reassurance that diving is safe and you can enjoy it, unfortunately flying to your dive trip is not fun and I recommend a very short prednisone taper to get you there. As far as hyperbaric treatment I think it’s very promising (but prohibitively expensive and inconvenient) and it is lacking a few elements that you can’t get without being submerged in water and I think those also might have a role in why it’s so successful..1 point
-
Interesting! Ironic that I was medically removed from the Navy's 2nd class(salvage) dive school due to cluster episodes. Might have been exactly what I needed the whole time! Been 15 years since my last episode but if they ever hit again I am headed to the local hyperbaric therapy center for a little experiment.1 point


.thumb.jpg.24dde7ef3152d6d31b9546e3fec3b26d.jpg)



.thumb.png.73f9ba561402bcb5b70c18f4f5dfd61f.png)
.thumb.png.cec58e020ae25568c83382a412ee1c85.png)
.thumb.png.a3dec81d909a0d96fbdaf0f52d94f48a.png)
.thumb.png.0c2bad424ad5aa48bbce3ce7227362d3.png)
.thumb.png.d188ab319301fbb908d26ead456aeff9.png)
.thumb.png.a8d24c252cc92d37b2b1662e52d4cea3.png)
.thumb.png.a3cc69db9a06a2b1177860efee95cd88.png)
.thumb.png.f95b30446ff53863045ef9ad8a47dda1.png)